Introduction:
The probability of maintaining treatment-free remission (TFR) after the discontinuation of tyrosine kinase inhibitors (TKI) is affected by clinical factors such as length of TKI treatment and the depth of molecular response. However, some individuals with similar treatment duration and response remain in TFR while others relapse. Thus, patient-specific factors must also play a role. Biological factors suggested to influence TFR include BCR::ABL1 transcript type, blasts at diagnosis, halving time (HT, first 3 months), BCR::ABL1 positivity at stop, and presence of somatic mutations.
The aim of this study was to evaluate the biological factors associated with TFR in the clinical practice, using data from the Canarian CML Registry.
Methods:
The OMOP-standardized data of adult patients with chronic phase CML who discontinued TKI treatment included in the Canarian CML Registry (https://rclmc.es/rclmc/) were reviewed.
Criteria to discontinue included TKI treatment ≥5 years and MR4.5 or better ≥3 years. TFR was defined as major molecular response (MMR), or deeper after stop. Molecular relapse was defined as loss of MMR in two consecutive tests.
NGS was performed with the 30-gene panel Myeloid Solution (SOPHiA) on the MiSeq (Illumina) platform using 200 ng genomic DNA extracted from peripheral blood at diagnosis.
Results:
A total of 109 patients were included, with an average age of 50.5 years; 54 were male (49.5%). Median follow-up was 3.3 years.
86 patients discontinued from first-line, 21 from second- and 2 from third-line. 51% of patients (n=56) discontinued from imatinib, 31% from nilotinib (n=34), 16% from dasatinib (n=17), and 1% from bosutinib and ponatinib (1 patient each).
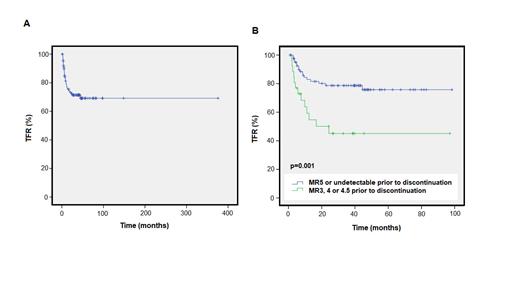
The median TFR was 101 months ( Figure 1A; range 1.02-148.4 months). Thirty-two patients had molecular relapse and re-started TKI treatment: 36.7% with imatinib or dasatinib, 26.7% with nilotinib. Median time to regain MMR was 101 days (range 25-276). No difference was observed in the time to regain MMR for imatinib vs. 2G-TKI (106 vs. 144, p=0.419). No patients progressed to an accelerated phase.
Differences were observed in duration of MR4 and MR4.5 prior to stop comparing the TFR vs. relapse groups (88.3 vs. 69.9 months, p=0.044; 74.2 vs. 58.6 months, p=0.079), but not total time on TKI (172.6 vs. 102.1, p=0.310), respectively.
In terms of biological factors at diagnosis, 44 patients had blasts, 66.7% had a low Sokal risk. 23.9% expressed transcript e13a2 and 76.1% had e14a2. No differences in TFR were observed when blasts, Sokal or transcript were considered in chi-squared analyses. A long HT (>21.9 days, Shanmuganathan et al. Blood 2021;137) was of marginal significance for molecular relapse (p=0.076, OR 3.2) but no difference was found for short HT (<9.4 days).
By Kaplan-Meier analysis, an MR3, 4, or 4.5 at stop was predictive of molecular relapse (n=42; Figure 1B) vs. an MR5 or undetectable (limit of detection 0.0001%). In multivariable analysis, only an MR5 or deeper at stop and withdrawal syndrome were predictive for TFR (p=0.003, HR 4.3; p=0.049, HR 0.20, respectively).
NGS data was available for 47 patients. Myeloid mutations were detected in 21 patients (44.7%) at diagnosis, of these 11 had an epigenetic mutation (23.9%; in ASXL1, DNMT3A, TET2 or EZH2). 11 patients (23.9%) had a variant that was potentially germline (VAF 40-60%).
By chi-squared and Kaplan-Meier analysis, no differences were observed between the median TFR for patients with or without a pathogenic somatic, epigenetic, ASXL1 or germline mutation. However, a greater separation of the curves was observed when considering TFR at 36 months for somatic (p=0.101) but not germline mutation.
Conclusions:
We confirmed previous observations that the biological factors BCR::ABL1 positivity at stop and longer HT were associated with molecular relapse although no difference was found for short HT.
The impact of clinical factors on TFR, including duration of MR4 and MR4.5 prior to stop, were also confirmed in our real-life series with a long follow-up, while total TKI duration was not prognostic.
Adnan Awad et al. associated the presence of epigenetic mutations at diagnosis with shorter TFR and higher relapse probability (Blood Cancer J. 2022;12). Here, a significant difference in TFR was not observed for epigenetic mutation at diagnosis; however, a tendency was observed between a pathogenic somatic but not a germline myeloid mutation and TFR at 36 months.
Disclosures
Stuckey:Gilead: Other: travel expenses; Novartis: Other: travel expenses. Segura-Díaz:Sanofi Genzyme: Honoraria; Novartis: Honoraria. Lakhwani:Janssen: Honoraria, Membership on an entity's Board of Directors or advisory committees; Novartis: Honoraria; Pfizer: Membership on an entity's Board of Directors or advisory committees. Bilbao-Sieyro:Abbvie: Honoraria. Gómez-Casares:Astellas: Research Funding; Incyte: Research Funding; AbbVie: Consultancy, Membership on an entity's Board of Directors or advisory committees; GSK: Consultancy, Membership on an entity's Board of Directors or advisory committees; Novartis: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding; Pfizer: Consultancy, Membership on an entity's Board of Directors or advisory committees; Amgen: Research Funding; Gilead: Other: Training support; Janssen: Other: Training support; AstraZeneca: Other: Training support.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal